Health & Wellness

You may have heard the term “pelvic floor” and brushed it off – thinking, I don’t need to know about that! But ignoring these muscles can lead to incontinence or pelvic organ prolapse. Take a step-by-step walk-through pelvic floor 101.
What is the pelvic floor?
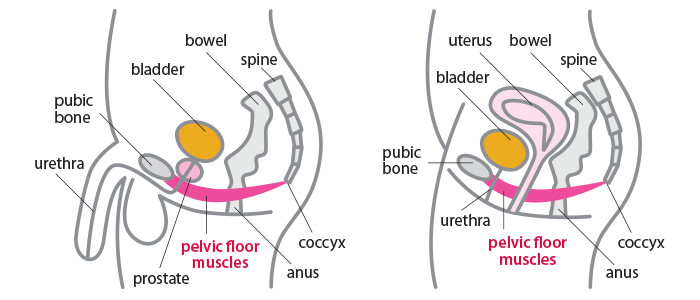
At times, it may feel like we are from different planets, but in this case, we are the same! Both men and women have a pelvic floor that consists of muscles, ligaments, connective tissues, and nerves:
- In women, it supports the bladder, uterus, vagina, and bowels and helps these pelvic organs function.
- In men, the pelvic floor supports the bladder and bowels.
Think of the pelvic floor muscles much like a hammock – the muscles stretch from the tailbone (coccyx) to the pubic bone (front to back) and from one sitting bone to the other (side to side). These muscles are normally firm and thick.
But this hammock can also act like a trampoline. The ligaments, muscles, and fascia need to provide the right amount of tension so the pelvic floor can move down and up – similar to springs on a trampoline.
Pelvic floor disorders occur when the trampoline or hammock that supports the pelvic organs becomes weak or damaged. The three most common pelvic floor disorders are:
- Urinary incontinence, or the involuntary leakage of urine.
- Fecal incontinence, or lack of bowel control.
- Pelvic organ prolapse, such as rectal prolapse, a condition in which the bowel can bulge through the anus.

Read stories from our Pelvic Floor Physical Therapy patients!
Memorial offers a Pelvic Floor Physical Therapy program led by Kylie Hayes-Akers, PT, DPT. Kylie is a pelvic floor therapist who is trained through the American Physical Therapy Association. Our program offers personalized, one-on-one physical therapy sessions in a private setting tailored to your symptoms and health goals. To schedule an evaluation, ask your doctor for a referral.
Five Important Roles Pelvic Floor Muscles Play
• Organ Support
• Bone Support
• Sphincteric Function
• Sexual Function
• Circulation
What contributes to pelvic floor disorders?
Common risk factors for pelvic floor dysfunction include:
- Childbirth is one of the main causes of pelvic floor disorders. A woman’s risk tends to increase the more times she has given birth or with a third/fourth degree laceration.
- Having pelvic or prostate surgery can cause dysfunction, due to potential nerve damage to the pelvic floor, as well as damage of supporting tissues due to chronic intra-abdominal pressure.
- Those who are overweight or obese also have a greater risk for pelvic floor disorders.
- Chronic constipation.
Are pelvic floor disorders a normal part of aging?
They can become more common as we get older, but they are not a normal or acceptable part of aging. These problems can have a significant impact on a person’s quality of life. Fortunately, these disorders often can be reversed with pelvic floor physical therapy.
What does pelvic floor physical therapy do?
Although the pelvic floor is hidden from view, it can be consciously controlled and therefore trained, much like our arm, leg, or abdominal muscles.
Treatments can include a wide range of therapies, such as manual therapy and therapeutic exercise techniques, in addition to electromyography (EMG) biofeedback and behavior/lifestyle modifications.
Take our quick 10-question quiz below!
Pelvic Health Quiz
Answer YES or NO to the following and learn if you have pelvic floor dysfunction:
- I sometimes have pelvic pain (in genitals, perineum, pubic or bladder area, or pain with urination) that exceeds a “3” on a 1-10 pain scale, with 10 being the worst pain imaginable.
- I can remember falling onto my tailbone, lower back, or buttocks (even in childhood).
- I sometimes experience one or more of the following urinary symptoms:
• Accidental loss of urine.
• Feeling unable to completely empty my bladder.
• Having to void within a few minutes of a previous void.
• Pain or burning with urination.
• Difficulty starting or frequent stopping/starting of urine stream. - I often or occasionally have to get up to urinate two or more times at night.
- I sometimes have a feeling of increased pelvic pressure or the sensation of my pelvic organs slipping down or falling out.
- I have a history of pain in my low back, hip, groin, or tailbone or have had sciatica.
- I sometimes experience one or more of the following bowel symptoms:
• Loss of bowel control.
• Feeling unable to completely empty my bowels.
• Straining or pain with a bowel movement.
• Difficulty initiating a bowel movement. - I sometimes experience pain or discomfort with sexual activity or intercourse.
- Sexual activity increases one or more of my other symptoms.
- Prolonged sitting increases my symptoms.
If you answered YES to three or more of the above, you are likely experiencing pelvic floor dysfunction. Speak to your physician about a referral to the Memorial Pelvic Floor Physical Therapy team to set up an appointment.
*The Cozean Questionnaire was created by Nicole Cozean, PT, DPT, WCS, CSCS* and Jesse Cozean, MBA.



